When fat gathers around the middle, it is more than a body image concern. It is often a sign that metabolism, hormones, blood sugar, or inflammation are out of balance.
At Kairos Health Integrative Primary Care, we pay close attention to changes in the waist and abdomen because they tell us what may be happening inside long before lab results become alarming.
This guide will help you understand what belly fat really is, why it develops, what risks come with ignoring it, and how we help patients turn things around using an evidence-based approach.
What Exactly Is Belly Fat?
Not all body fat is the same. The soft layer you can pinch under the skin is called subcutaneous fat.
The deeper fat that collects inside the abdomen around organs like the liver, pancreas, and intestines is called visceral fat.
That deeper visceral fat is the main culprit behind metabolic problems. It behaves differently. It sends out inflammatory signals, changes how your body uses insulin, and can raise cholesterol and blood pressure.
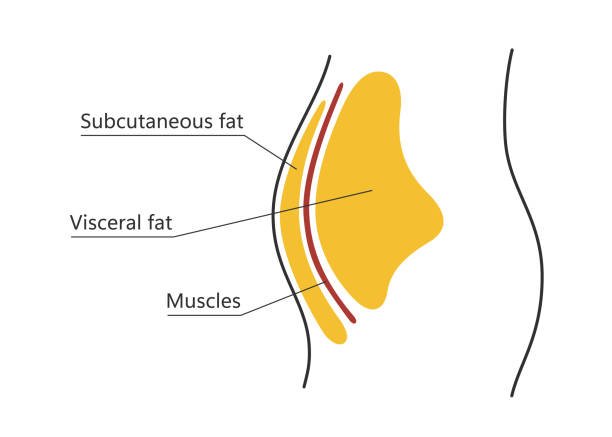
So when we talk about belly fat in a clinical sense, we are often talking about visceral fat and the metabolic stress that goes with it.
When Should You Be Concerned About Your Waist?
Take a moment and consider these questions:
- Has my waist measurement increased over the past year, even if my scale weight has not?
- Do I gain most of my weight around the middle rather than the hips or thighs?
- Do I often feel bloated or puffy in my stomach after meals?
- Have I been told I have high triglycerides, elevated fasting insulin, prediabetes, or fatty liver?
- Do I crash after eating carbohydrates or feel better when I include protein and fiber?
- Have I had major hormone changes (perimenopause, low testosterone, PCOS) that are linked to my waistline?
If several answers are yes, it is worth taking a closer look at what your body is trying to tell you.
Why Belly Fat Builds Up?
Belly fat does not happen overnight, and it is not always about eating too much. Here are patterns we frequently uncover during a checkup..
Insulin Resistance
When cells stop responding properly to insulin, the body produces more of it. High insulin promotes fat storage in the abdomen. Many people develop insulin resistance years before their blood sugar moves out of range, which is why early testing matters..
Stress and Cortisol
Your body treats chronic stress like a survival event. Cortisol rises, blood sugar fluctuates, and the signal to store energy (especially centrally) becomes stronger. Long workdays, poor boundaries, and tense sleep all feed this loop.
Hormone Shifts
Low thyroid, estrogen changes in perimenopause, low testosterone in men, or high androgens in PCOS can all shift fat storage toward the belly. Hormones guide where and how the body holds weight.
Food Quality and Refined Carbs
High intake of sweetened drinks, refined grains, and ultra‑processed foods drives blood sugar swings and fat production in the liver. Over time, this promotes visceral fat and inflammation.
Sleep Debt
Less than seven hours of quality sleep raises appetite hormones, increases sugar cravings, and reduces insulin sensitivity. Many patients see a measurable waist change after improving sleep.
Movement Gaps
You do not need extreme workouts, but long periods of sitting reduce glucose uptake by muscle and encourage fat storage. Short bursts of movement across the day make a difference.
Health Risks Linked to Belly Fat
Visceral fat is active tissue. It produces inflammatory chemicals, sends fatty acids to the liver, and disrupts hormone and insulin balance.
Over time, this raises the risk for several conditions.
Type 2 diabetes and prediabetes: Belly fat and insulin resistance are strongly connected. The more central fat you have, the harder it becomes for your body to manage blood sugar effectively.
Heart disease and stroke: Belly fat is often linked to high triglycerides, low HDL, and vascular inflammation, all of which increase the risk of heart disease.
High blood pressure: Visceral fat contributes to the stiffening of blood vessels and fluid imbalance, which can cause elevated blood pressure over time.
Fatty liver disease: When too much fat is sent to your liver, it begins to store fat instead of processing it properly, leading to liver inflammation and scarring if not addressed.
Hormonal disruption: Extra belly fat can disrupt key hormones. This can cause issues like PCOS, low testosterone in men, irregular menstrual cycles, and estrogen changes during menopause.
Cognitive decline: Visceral fat can affect brain function and increase the risk of memory problems later in life.
Even a slight rise in waist size can lead to higher long‑term risk, which is why we track it along with labs.
How To Measure Your Waist Correctly
Accurate measurement matters. Use a soft tape measure. Stand tall, relax your abdomen, and find the midpoint between the bottom of your ribs and the top of your hip bones. Wrap the tape level around your bare skin. Exhale gently and read the number without pulling tight.

Look for:
- Women: 35 inches (88 cm) or above suggests increased metabolic risk.
- Men: 40 inches (102 cm) or above suggests increased metabolic risk.
These are general guides, not personal verdicts. Some people with smaller waists still carry metabolic risk if insulin, liver function, or hormones are imbalanced.
That is why we combine measurement with lab and symptom review.
What We Look at Kairos
When someone comes to Kairos Integrative Care concerned about belly fat or a growing waist, we do not jump straight to eating less. We look for what is driving this change.
We may review:
Metabolic labs: Fasting glucose, fasting insulin, and an insulin resistance score help us see early changes.
Lipid panel: Triglycerides, HDL, and sometimes advanced particles give insight into fat transport and cardiovascular risk.
Liver enzymes: Elevated ALT or GGT may point toward fatty liver linked to abdominal fat gain.
Hormones: Thyroid function, sex hormones, and in some cases, cortisol patterns explain shifts in fat distribution.
Inflammation markers: High‑sensitivity CRP or other markers show whether inflammation is part of the picture.
Body composition tools: When available, bioimpedance or DEXA scans help differentiate fat from lean tissue and show visceral fat trends.
Stress, Sleep, and Your Waist
If your belly grew during a stressful period, shift work, or months of poor sleep, it’s not your imagination.
Stress hormones make your body store more fat around the waist and make it harder to control hunger and blood sugar.
Improving sleep, creating a relaxing evening routine, and using simple stress resets like deep breathing or light movement can help calm these hormonal effects and support a healthier waistline.
When To Get Help
Consider booking a visit if:
- Your waist keeps growing, and you do not know why.
- Lab tests have shown high triglycerides, prediabetes, or fatty liver.
- You have PCOS, thyroid issues, or unexplained weight shifts.
- You feel inflamed, puffy, or tired after meals.
- Lifestyle changes are not moving the needle, and you want targeted guidance.
Early action reduces the risks of long-term health problems.
Conclusion
If your waist is getting bigger or belly fat is a concern, you don’t have to figure it out on your own
At Kairos, Lola, one of our Board‑Certified Nurse Practitioners, reviews your history, runs the right labs, and helps create a plan that works with your real life.
Whether your next step is balancing blood sugar, checking hormones, supporting liver health, or rebuilding sleep, we guide you through it.
We see patients in Houston, Sugar Land, and nearby areas (77046 and 77478) and accept most major insurance plans, including Aetna, Cigna, BCBS, UnitedHealthcare, Tricare, and more.
Book your appointment today!




